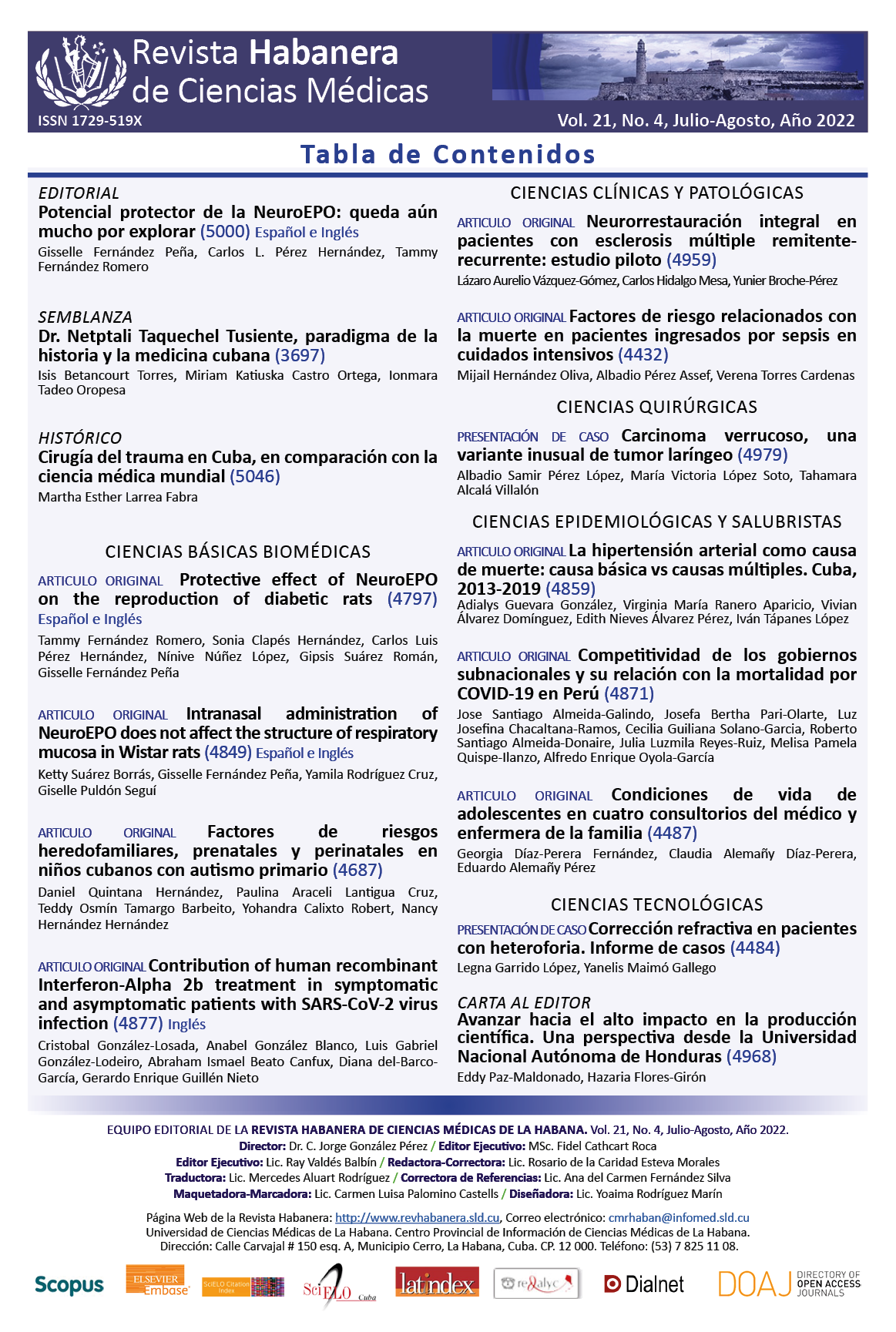
Contribución del tratamiento con Interferón-Alpha 2b humano recombinante en pacientes sintomáticos y asintomáticos con infección por el virus SARS-CoV2
Palabras clave:
; SARS-CoV-2; interferón tipo I; COVID-19; Heberon®; relación neutrófilos / linfocitos; pacientes asintomáticos con COVID-19.Resumen
Introducción: Los sujetos con infección asintomática generalmente no son admitidos en centros de asistencia médica, sin embargo, pueden beneficiarse de la terapia antiviral.
Objetivo: evaluar la contribución al tratamiento de la terapia combinada basada en interferón alfa 2b recombinante humano + Lopinavir/Ritonavir + Cloroquina contra Lopinavir/Ritonavir + Cloroquina en pacientes asintomáticos y sintomáticos.
Material y Métodos: Se realizó un estudio observacional en pacientes con diagnóstico positivo de COVID-19, durante los días del 1 de abril al 30 de julio de 2020. De un total de 308 pacientes tratados con interferón + Lopinavir/Ritonavir + Cloroquina, se seleccionaron mediante un proceso de aleatorización simple, una muestra estadísticamente representativa de 40 pacientes. Como grupo control se seleccionaron 27 pacientes que solo recibieron tratamiento con Lopinavir/Ritonavir + Cloroquina. Estos pacientes se sometieron a determinaciones de anticuerpos anti-SARS-CoV-2, determinaciones de marcadores inflamatorios y seguimiento por RT-PCR para evaluar el tiempo de negativización.
Resultados: El grupo tratado con interferón tuvo un tiempo significativamente más corto de negativización. Los pacientes tratados con interferón mostraron una disminución significativa de los marcadores inflamatorios en el momento del alta hospitalaria y tuvieron un incremento de los títulos de anticuerpos a los dos y cuatro meses posteriores al alta hospitalaria, en comparación con el grupo de pacientes que no recibió interferón.
Conclusiones: El tratamiento con interferón exógeno en pacientes con COVID-19 tuvo una contribución significativa en la regulación de la respuesta inmune de los pacientes.
Descargas
Citas
1. Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19). Int J Antimicrob Agents [Online]. 2020;55(3):105924. Available from: https://doi.org/10.1016/j.ijantimicag.2020.105924
2. World Health Organization. Coronavirus disease 2019 (COVID-19) [Online]. Geneva: World Health Organization; 2020 [Cited 13/02/2022]. Available from: https://www.covid19.who.int
3. García LF. Immune Response, Inflammation, and the Clinical Spectrum of COVID-19. Front Immunol [Online]. 2020;11(1441):[Aprox. 2p.]. Available from: https://doi.org/10.3389/fimmu.2020.01441
4. Pereda R, González D, Rivero HB, Rivero JC, Pérez A, López LDR, et al. Therapeutic Effectiveness of Interferon-α2b Against COVID-19: The Cuban Experience. Journal Interferon Cytokine Research [Online]. 2020;40(9):438-42. Available from: https://doi.org/10.1089/jir.2020.0124
5. Ministerio de Salud Pública. Protocolo de actuación nacional para la COVID-19 [Online]. La Habana: MINSAP; 2020 [Cited 13/02/2022]. Available from: https://www.mined.gob.cu/protocolo-de-actuacion-nacional-para-la-516covid-19-en-cuba-pdf/
6. World Health Organization. Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: interim guidance, 28 January 2020 [Online]. Geneva: World Health Organization; 2020 [Cited 13/02/2022]. Available from: https://www.who.int/docs/default-source/coronaviruse/clinical-management-of-novel-cov.pdf
7. Barboza JJ, Chambergo Michilot D, Velasquez Sotomayor M, Silva Rengifo C, Diaz Arocutipa C, Caballero Alvarado J, et al. Assessment and management of asymptomatic COVID-19 infection: A systematic review. Travel Med Infect Dis [Online]. 2021;41:102058. Available from: https://doi.org/10.1016/j.tmaid.2021.102058
8. Laboratory Guidelines for Detection and Diagnosis of the Novel Coronavirus (2019-nCov) Infection [Online]. Geneva: WHO; 2020 [Cited 13/02/2022]. Available from: https://www.paho.org/en/documents/laboratory-guidelines-detection-and-diagnosis-novel-coronavirus-2019-ncov-infection
9. Declaración de Helsinki de la AMM - Principios éticos para las investigaciones médicas en seres humanos [Online]. EE UU: WMA; 2017. [Cited 13/02/2022]. Available from: http://www.wma.net/es/30publications/10policies/b3/index.html
10. Centers for Disease Control and Prevention. Clinical Care Quick Reference for COVID-19 [Online]. Atlanta: CDCP ; 2021 [Cited 13/02/2022]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care-quick-reference.html
11. Ali RMM, Ghonimy MBI. Radiological findings spectrum of asymptomatic coronavirus (COVID-19) patients. Egyptian Journal of Radiology and Nuclear Medicine [Online]. 2020;51(1):156. Available from: https://doi.org/10.1186/s43055-020-00266-3
12. Nishiura H, Kobayashi T, Miyama T, Suzuki A, Jung SM, Hayashi K, et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19). Int J Infect Dis [Online]. 2020;94:154-5. Available from: https://doi.org/10.1016/j.ijid.2020.03.020
13. Chan YH, Fong SW, Poh CM, Carissimo G, Yeo NK, Amrun SN, et al. Asymptomatic COVID-19: disease tolerance with efficient anti-viral immunity against SARS-CoV-2. EMBO Molecular Medicine [Online]. 2021;13(6):e14045. [Cited 13/02/2022]. Available from: https://europepmc.org/article/MED/33961735
14. Cruz LR, Baladrón I, Rittoles A, Díaz PA, Valenzuela C, Santana R, et al. Treatment with an Anti-CK2 Synthetic Peptide Improves Clinical Response in COVID-19 Patients with Pneumonia. A Randomized and Controlled Clinical Trial. ACS Pharmacology Translational Science [Online]. 2021;4(1):206-12. Available from: https://doi.org/10.1021/acsptsci.0c00175
15. Long QX, Tang XJ, Shi QL, Li Q, Deng HJ, Yuan J, et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nature Medicine [Online]. 2020;26(8):1200-4. Available from: https://doi.org/10.1038/s41591-020-0965-6
16. Garcia del Barco D, Risco Acevedo D, Berlanga Acosta J, Martos Benítez FD, Guillén Nieto G. Revisiting Pleiotropic Effects of Type I Interferons: Rationale for Its Prophylactic and Therapeutic Use Against SARS-CoV-2. Front Immunol [Online]. 2021;12(875):[Aprox. 2p.]. Available from: https://doi.org/10.3389/fimmu.2021.655528
17. Channappanavar R, Fehr AR, Vijay R, Mack M, Zhao J, Meyerholz DK, et al. Dysregulated Type I Interferon and Inflammatory Monocyte-Macrophage Responses Cause Lethal Pneumonia in SARS-CoV-Infected Mice. Cell Host Microbe [Online]. 2016;19(2):181-93. Available from: https://doi.org/10.1016/j.chom.2016.01.007
18. Park A, Iwasaki A. Type I and Type III Interferons - Induction, Signaling, Evasion, and Application to Combat COVID-19. Cell Host Microbe [Online]. 2020;27(6):870-8. Available from: https://doi.org/10.1016/j.chom.2020.05.008
19. Wu R, Wang L, Kuo HCD, Shannar A, Peter R, Chou PJ, et al. An Update on Current Therapeutic Drugs Treating COVID-19. Curr Pharmacol Rep [Online]. 2020:1-15. Available from: https://doi.org/10.1007/s40495-020-00216-7
20. Lam S, Lombardi A, Ouanounou A. COVID-19: A review of the proposed pharmacological treatments. Eur J Pharmacol [Online]. 2020;886:173451. Available from: https://doi.org/10.1016/j.ejphar.2020.173451
21. Lokugamage KG, Hage A, Schindewolf C, Rajsbaum R, Menachery VD. SARS-CoV-2 is sensitive to type I interferon pretreatment [Online]. New York: BioRxiv; 2020. Available from: https://doi.org/10.1101/2020.03.07.982264
22. Zhou Q, Chen V, Shannon CP, Wei XS, Xiang X, Wang X, et al. Interferon-α2b Treatment for COVID-19. Front Immunol [Online]. 2020;11(1061):[Aprox. 2 p.]. Available from: https://doi.org/10.3389/fimmu.2020.01061
23. Pandit A, Bhalani N, Bhushan BLS, Koradia P, Gargiya S, Bhomia V, et al. Efficacy and safety of pegylated interferon alfa-2b in moderate COVID-19: A phase II, randomized, controlled, open-label study. Int J Infect Dis [Online]. 2021;105:516-23. Available from: https://doi.org/10.1016/j.ijid.2021.03.015
24. Ghazy RM, Almaghraby A, Shaaban R, Kamal A, Beshir H, Moursi A, et al. A systematic review and meta-analysis on chloroquine and hydroxychloroquine as monotherapy or combined with azithromycin in COVID-19 treatment. Sci Rep [Online]. 2020;10(1):22139. Available from: https://doi.org/10.1038/s41598-020-77748-x
25. Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, et al. A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19. N Engl J Med [Online]. 2020;382(19):1787-99. Available from: https://doi.org/10.1056/NEJMoa2001282
26. Fricke Galindo I, Falfán Valencia R. Genetics Insight for COVID-19 Susceptibility and Severity: A Review. Front Immunol [Online]. 2021;12(1057):[Aprox. 2p.]. Available from: https://doi.org/10.3389/fimmu.2021.622176
27. Mantlo E, Bukreyeva N, Maruyama J, Paessler S, Huang C. Antiviral activities of type I interferons to SARS-CoV-2 infection. Antiviral Res [Online]. 2020;179:104811. Available from: https://doi.org/10.1016/j.antiviral.2020.104811
28. Hadjadj J, Yatim N. Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science [Online]. 2020;369(6504):718-24. Available from: https://doi.org/10.1126/science.abc6027
29. Blanco Melo D, Nilsson Payant BE, Liu WC, Uhl S, Hoagland D, Møller R, et al. Imbalanced Host Response to SARS-CoV-2 Drives Development of COVID-19. Cell [Online]. 2020;181(5):1036-45.e9. Available from: https://doi.org/10.1016/j.cell.2020.04.026
30. Hung IF, Lung KC, Tso EY, Liu R, Chung TW, Chu MY, et al. Triple combination of interferon beta-1b, lopinavir-ritonavir, and ribavirin in the treatment of patients admitted to hospital with COVID-19: an open-label, randomised, phase 2 trial. Lancet [Online]. 2020;395(10238):1695-704. Available from: https://doi.org/10.1016/S0140-6736(20)31042-4
31. Acharya D, Liu G, Gack MU. Dysregulation of type I interferon responses in COVID-19. Nat Rev Immunol [Online]. 2020;20(7):397-8. Available from: https://doi.org/10.1038/s41577-020-0346-x
32. Mehmood I, Ijaz M, Ahmad S, Ahmed T, Bari A, Abro A, et al. SARS-CoV-2: An Update on Genomics, Risk Assessment, Potential Therapeutics and Vaccine Development. Int J Environ Res Public Health [Online]. 2021;18(4):1626. Available from: https://doi.org/10.3390/ijerph18041626
33. Nakhlband A, Fakhari A, Azizi H. Interferon-alpha position in combating with COVID-19: A systematic review. J Med Virol [Online]. 2021. 93(9):5277-84. Available from: https://doi.org/10.1002/jmv.27072
34. Meng Z, Wang T, Chen L, Chen X, Li L, Qin X, et al. The Effect of Recombinant Human Interferon Alpha Nasal Drops to Prevent COVID-19 Pneumonia for Medical Staff in an Epidemic Area. Current Topics Medicinal Chemistry [Online]. 2021; 21(10):[Aprox. 2p.]. Available fom: https://dx.doi.org/10.2174/1568026621666210429083050
35. Shalhoub S, Farahat F, Al Jiffri A, Simhairi R, Shamma O, Siddiqi N, et al. IFN-α2a or IFN-β1a in combination with ribavirin to treat Middle East respiratory syndrome coronavirus pneumonia: a retrospective study. J Antimicrob Chemother [Online]. 2015;70(7):2129-32. Available from: https://doi.org/10.1093/jac/dkv08536
36. Fritsch SD, Weichhart T. Effects of Interferons and Viruses on Metabolism. Front Immunol [Online]. 2016;7(630)[Aprox. 2p.]. Available from: https://doi.org/10.3389/fimmu.2016.00630
37. Imran MM, Ahmad U, Usman U, Ali M. Neutrophil/lymphocyte ratio-A marker of COVID-19 pneumonia severity. Int J Clin Pract [Online]. 2021;75(4):e13698. Available from: https://doi.org/10.1111/ijcp.13698
38. Xia X, Wen M, Zhan S, He J, Chen W. An increased neutrophil/lymphocyte ratio is an early warning signal of severe COVID-19. Nan fang yi ke da xue xue bao = Journal of Southern Medical University [Online]. 2020;40(3):333-6. Available from: https://doi.org/10.12122/j.issn.1673-4254.2020.03.06
39. Fei M, Tong F, Tao X, Wang J.Value of neutrophil-to-lymphocyte ratio in the classification diagnosis of coronavirus disease 2019. Zhonghua wei zhong bing ji jiu yi xue [Online]. 2020;32(5):554-8. Available from: https://doi.org/10.1186/s13054-020-03374-8
40. Li X, Liu C, Mao Z, Xiao M, Wang L, Qi S, et al. Predictive values of neutrophil-to-lymphocyte ratio on disease severity and mortality in COVID-19 patients: a systematic review and meta-analysis. Crit Care [Online]. 2020;24(1):647. Available from: https://doi.org/10.1186/s13054-020-03374-8
41. Stam TC, Swaak AJ, Kruit WH, Eggermont AM. Regulation of ferritin: a specific role for interferon-alpha (IFN-alpha)? The acute phase response in patients treated with IFN-alpha-2b. Europ J Clin Invest [Online]. 2002;32(1):79-83. Available from: https://doi.org/10.1046/j.1365-2362.2002.0320s1079.x
42. Ladero JM, López Alonso G, Devesa MJ, Cuenca F, Ortega L, Agreda M, et al. Oscillations in serum ferritin associated with antiviral therapy in chronic hepatitis C. Rev Esp Enferm Dig [Online]. 2009 [Cited 13/02/2022];101:31-40. Available from: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1130-01082009000100004&lng=en
43. Grzelak L, Temmam S. A comparison of four serological assays for detecting anti-SARS-CoV-2 antibodies in human serum samples from different populations. Sci Transl Med [Online]. 2020;12(559):eabc3103. Available from: https://doi.org/10.1126/scitranslmed.abc3103
44. Dufloo J, Grzelak L, Staropoli I, Madec Y, Tondeur L, Anna F, et al. Asymptomatic and symptomatic SARS-CoV-2 infections elicit polyfunctional antibodies. Cell Rep Med [Online]. 2021;2(5):100275. Available from https://doi.org/10.1016/j.xcrm.2021.100275
45. Centers for Disease Control and Prevention. Antibodies and the immune system [Online]. Atlanta: CDCP; 2021 [Cited 13/02/2022]. Available from: https://espanol.cdc.gov/coronavirus/2019-ncov/your-health/about-covid-19/antibodies.html
46. Tough DF. Type I Interferon as a Link Between Innate and Adaptive Immunity through Dendritic Cell Stimulation. Leuk Lymphoma [Online]. 2004;45(2):257-64. Available from: https://doi.org/10.1080/1042819031000149368
47. Huber JP, Farrar JD. Regulation of effector and memory T-cell functions by type I interferon. Immunology [Online]. 2011;132(4):466-74. Available from: https://doi.org/10.1111/j.1365-2567.2011.03412.x
48. Peng Y, Mentzer AJ. Broad and strong memory CD4(+) and CD8(+) T cells induced by SARS-CoV-2 in UK convalescent individuals following COVID-19. Nat Immunol [Online]. 2020;21(11):1336-45. Available from: https://doi.org/10.1038/s41590-020-0782-6