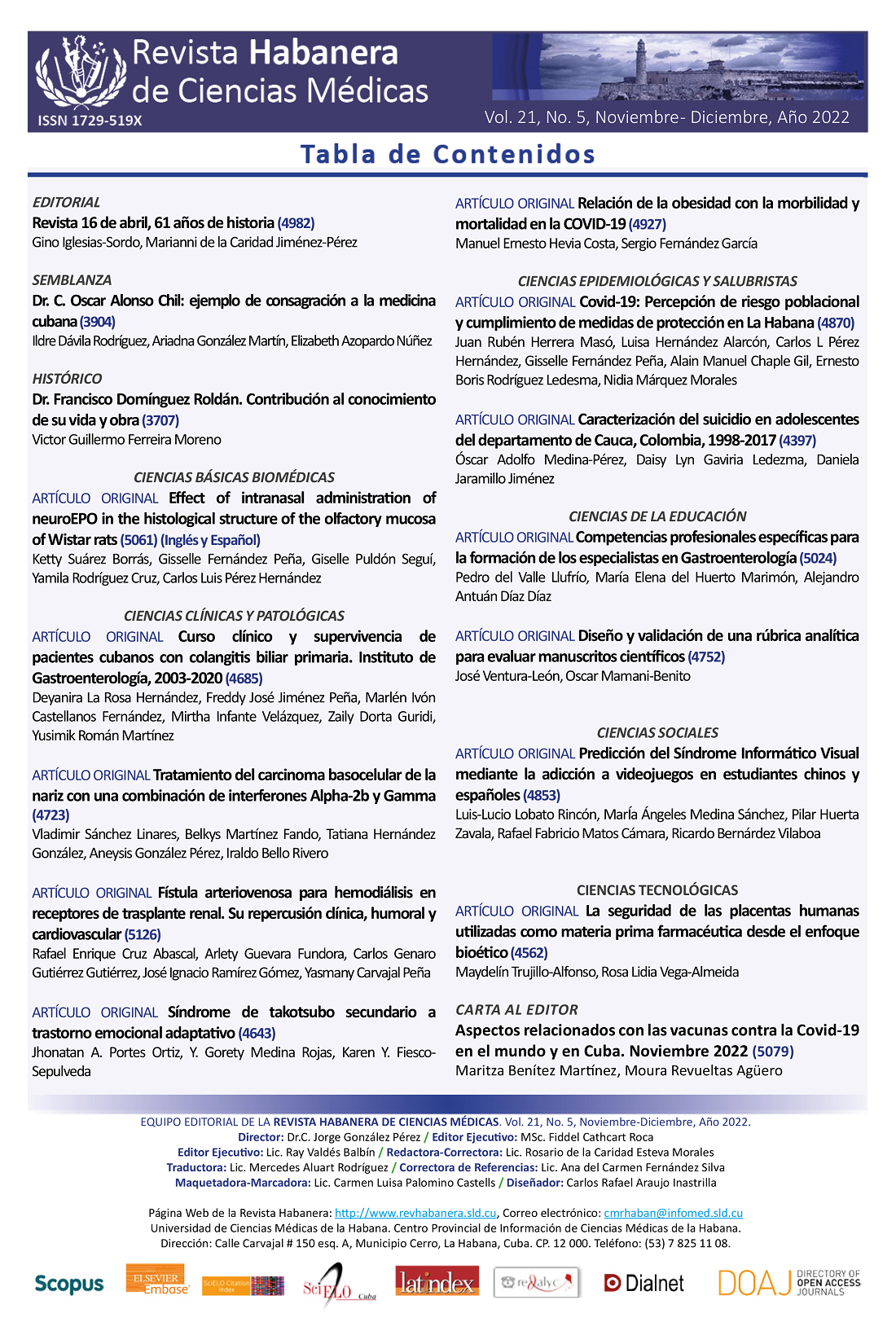
Efecto de la administración intranasal de NeuroEPO en la estructura histológica de la mucosa olfatoria de ratas Wistar
Palabras clave:
NeuroEPO, Eritropoyetina, mucosa olfatoria, administración intranasal, enfermedades neurodegenerativas, neuroprotección.Resumen
Introducción: Los accidentes cerebrovasculares y las enfermedades neurodegenerativas constituyen un importante problema de salud mundial. No solo porque causan una alta mortalidad y discapacidad, sino por la falta de terapias eficaces para tratarlos. La NeuroEPO, una variante de la eritropoyetina humana recombinante (rHu-EPO) con bajo contenido en ácido siálico, ha mostrado resultados alentadores como potencial agente neuroprotector al ser administrada por vía intranasal.
Objetivo: Determinar el efecto de la administración intranasal de NeuroEPO en la estructura histológica de la mucosa olfatoria de ratas Wistar.
Materiales y Métodos: Se realizó un estudio experimental, prospectivo y de corte longitudinal en ratas Wistar. Se utilizaron diez animales sanos distribuidos aleatoriamente en dos grupos de cinco cada uno. El grupo control recibió vehículo (0,3 μl/g/día) y el grupo tratado recibió NeuroEPO (300 μg/kg/día). Ambos tratamientos fueron administrados por vía intranasal durante 28 días. Fueron evaluadas las características histológicas de la mucosa olfatoria. Las medianas de los grupos del estudio fueron comparadas mediante la prueba U de Mann-Whitney.
Resultados: No se evidenciaron alteraciones en las características histológicas del epitelio olfatorio. Sin embargo, a nivel de la lámina propia en el grupo tratado con NeuroEPO, se observó una ligera hipertrofia e hiperplasia de las glándulas de Bowman.
Conclusiones: La administración de la formulación nasal de NeuroEPO no indujo alteraciones histopatológicas de la mucosa olfatoria de ratas Wistar en las condiciones experimentales de esta investigación.Descargas
Citas
1. WHO. World health statistics 2022 (Monitoring health of the SDGs) [Internet]. 2022. 1–131 p. Available from: http://apps.who.int/bookorders.
2. Deuschl G, Beghi E, Fazekas F, Varga T, Christoforidi KA, Sipido E, et al. The burden of neurological diseases in Europe: an analysis for the Global Burden of Disease Study 2017. Lancet Public Health. 2020 Oct 1;5(10):e551–67.
3. Feigin VL, Vos T, Nichols E, Owolabi MO, Carroll WM, Dichgans M, et al. The global burden of neurological disorders: translating evidence into policy. Lancet Neurol. 2020 Mar 1;19(3):255–65.
4. Vittori DC, Chamorro ME, Hernández Y v., Maltaneri RE, Nesse AB. Erythropoietin and derivatives: Potential beneficial effects on the brain. J Neurochem [Internet]. 2021 Sep 1 [cited 2022 Oct 24];158(5):1032–57. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/jnc.15475
5. Rey F, Balsari A, Giallongo T, Ottolenghi S, di Giulio AM, Samaja M, et al. Erythropoietin as a Neuroprotective Molecule: An Overview of Its Therapeutic Potential in Neurodegenerative Diseases. https://doi.org/101177/1759091419871420 [Internet]. 2019 Aug 26 [cited 2022 Oct 24];11. Available from: https://journals.sagepub.com/doi/full/10.1177/1759091419871420
6. Garzón F, Coimbra D, Parcerisas A, Rodriguez Y, García JC, Soriano E, et al. NeuroEPO Preserves Neurons from Glutamate-Induced Excitotoxicity. Journal of Alzheimer’s Disease. 2018 Jan 1;65(4):1469–83.
7. Fernando G, Yamila R, Cesar GJ, Ramón R. Neuroprotective Effects of neuroEPO Using an In Vitro Model of Stroke [Internet]. Behavioral Sciences Multidisciplinary Digital Publishing Institute; Feb 13, 2018 p. 26. Available from: https://www.mdpi.com/2076-328X/8/2/26/htm
8. Maurice T, Mustafa MH, Desrumaux C, Keller E, Naert G, García-Barceló MDLC, et al. Intranasal formulation of erythropoietin (EPO) showed potent protective activity against amyloid toxicity in the Aβ25-35 non-transgenic mouse model of Alzheimer’s disease. https://doi.org/101177/0269881113494939 [Internet]. 2013 Jun 26 [cited 2022 Oct 24];27(11):1044–57. Available from: https://journals.sagepub.com/doi/abs/10.1177/0269881113494939
9. Cruz YR, Strehaiano M, Rodríguez Obaya T, Rodríguez JCG, Maurice T. An Intranasal Formulation of Erythropoietin (Neuro-EPO) Prevents Memory Deficits and Amyloid Toxicity in the APP Swe Transgenic Mouse Model of Alzheimer’s Disease. Journal of Alzheimer’s Disease. 2017 Jan 1;55(1):231–48.
10. Pérez L, Sosa S, Bringas G, López D, Valenzuela C, Peñalver AI, et al. NeuroEPO in mild-to-moderate Alzheimer’s disease. Alzheimer’s & Dementia [Internet]. 2020 Dec [cited 2022 Aug 8];16(S9):e036167. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/alz.036167
11. Bringas Vega ML, Pedroso Ibáñez I, Razzaq FA, Zhang M, Morales Chacón L, Ren P, et al. The Effect of Neuroepo on Cognition in Parkinson’s Disease Patients Is Mediated by Electroencephalogram Source Activity. Front Neurosci. 2022;0(June):952.
12. Santos-Morales O, Díaz-Machado A, Jiménez-Rodríguez D, Pomares-Iturralde Y, Festary-Casanovas T, González-Delgado CA, et al. Nasal administration of the neuroprotective candidate NeuroEPO to healthy volunteers: A randomized, parallel, open-label safety study. BMC Neurol [Internet]. 2017 Jul 4 [cited 2022 Aug 8];17(1):1–9. Available from: https://link.springer.com/articles/10.1186/s12883-017-0908-0
13. Pedroso I, Garcia M, Casabona E, Morales L, Bringas ML, Pérez L, et al. Protective Activity of Erythropoyetine in the Cognition of Patients with Parkinson’s Disease. Behavioral Sciences 2018, Vol 8, Page 51 [Internet]. 2018 May 21 [cited 2022 Oct 24];8(5):51. Available from: https://www.mdpi.com/2076-328X/8/5/51/htm
14. Rodriguez-Labrada R, Ortega-Sanchez R, Hernández Casaña P, Santos Morales O, Padrón-Estupiñan M del C, Batista-Nuñez M, et al. Erythropoietin in Spinocerebellar Ataxia Type 2: Feasibility and Proof-of-Principle Issues from a Randomized Controlled Study. Movement Disorders [Internet]. 2022 Jul 1 [cited 2022 Oct 24];37(7):1516–25. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/mds.29045
15. Fernández Romero T, Clapés Hernández S, Pérez Hernández CL, Barreto López JJ, Fernández Peña G, Fernández Romero T, et al. Efecto hipoglicemiante de la NeuroEPO en ratas con y sin diabetes mellitus. Revista Habanera de Ciencias Médicas [Internet]. 2022 [cited 2022 Aug 6];21(1). Available from: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1729-519X2022000100003&lng=es&nrm=iso&tlng=es
16. Fernández Romero T, Clapes Hernández S, Pérez Hernández CL, Núñez López N, Suárez Román G, Fernández Peña G. Protective effect of NeuroEPO on the reproduction of diabetic rats. Revista Habanera de Ciencias Médicas [Internet]. 2022 Sep 22 [cited 2022 Oct 13];21(4):4797. Available from: http://www.revhabanera.sld.cu/index.php/rhab/article/view/4797
17. Suárez Borrás K, Fernández Peña G, Rodríguez Cruz Y, Puldón Seguí G. Intranasal administration of NeuroEPO does not affect the structure of respiratory mucosa in Wistar rats. Revista Habanera de Ciencias Médicas [Internet]. 2022 Sep 22 [cited 2022 Oct 26];21(4):4849. Available from: http://www.revhabanera.sld.cu/index.php/rhab/article/view/4849
18. Couto M, Cates C. Laboratory Guidelines for Animal Care. In Humana, New York, NY; 2019 [cited 2020 Mar 30]. p. 407–30. Available from: http://link.springer.com/10.1007/978-1-4939-9009-2_25
19. McCormick-Ell J, Connell N. Laboratory Safety, Biosecurity, and Responsible Animal Use. ILAR J [Internet]. 2019 Aug 16 [cited 2020 Mar 30];60(1):24–33. Available from: https://academic.oup.com/ilarjournal/advance-article/doi/10.1093/ilar/ilz012/5550511
20. Muñoz Cernada A, García Rodríguez JC, Nuñez Figueredo Y, Pardo Ruiz Z, García Selman JD, Sosa Testé I, et al. Formulaciones nasales de EPORH con bajo contenido de ácido siálico para el tratamiento de enfermedades del sistema nervioso central [Internet]. 2007 [cited 2022 Oct 24]. Available from: https://patentscope.wipo.int/search/es/detail.jsf?docId=WO2007009404
21. Humason GL. Animal tissue techniques. [Internet]. Animal tissue techniques. San Francisco (& London): W. H. Freeman and Company; 1962 [cited 2022 Oct 26]. Available from: https://www.cabdirect.org/cabdirect/abstract/19622204447
22. Uraih LC, Maronpot RR. Normal histology of the nasal cavity and application of special techniques. Environ Health Perspect. 1990 Apr;85:187–208.
23. Kumar V, Abbas AbulK, Aster JonC. Robbins and Cotran Pathologic Basis of Disease [Internet]. 10th ed. Kumar V, K Singh M, editors. Elsevier. Philadelphia: Thomas press India Ltd, ,Elsevier Publication; 2018 [cited 2022 Oct 26]. Available from: https://www.elsevier.com/books/robbins-and-cotran-pathologic-basis-of-disease/kumar/978-0-323-53113-9
24. Suárez K, Fernández G, Puldón G, Rodriguez Y, Pérez CL. Effect of intranasal administration of neuroEPO in the histological structure of the olfactory mucosa of rats Wistar. [Internet]. Mendeley Data. Mendeley; [cited 2022 Oct 25]. Available from: https://data.mendeley.com/datasets/gc77wttd9h
25. Graff CL, Pollack GM. Nasal Drug Administration: Potential for Targeted Central Nervous System Delivery. J Pharm Sci. 2005 Jun 1;94(6):1187–95.
26. Keller LA, Merkel O, Popp A. Intranasal drug delivery: opportunities and toxicologic challenges during drug development. Drug Deliv Transl Res [Internet]. 2022 Apr 1 [cited 2022 Oct 26];12(4):735–57. Available from: https://link.springer.com/article/10.1007/s13346-020-00891-5
27. Lagarto A, Bueno V, Guerra I, Valdés O, Couret M, López R, et al. Absence of hematological side effects in acute and subacute nasal dosing of erythropoietin with a low content of sialic acid. Experimental and Toxicologic Pathology. 2011 Sep 1;63(6):563–7.
28. Kovalchuk Nataliia. ORGAN-SPECIFIC CONTRIBUTION OF P450 ENZYMES TO BIOACTIVATION AND ACUTE RESPIRATORY TRACT TOXICITY OF NAPHTHALENE by Nataliia Kovalchuk A Dissertation. New York : State University of New York ; 2017.
29. Cüreoǧlu S, Akkuş M, Osma Ü, Yaldiz M, Oktay F, Can B, et al. The effect of benzalkonium chloride on rabbit nasal mucosa in vivo: an electron microscopy study. European Archives of Oto-Rhino-Laryngology 2002 259:7 [Internet]. 2002 [cited 2022 Oct 26];259(7):362–4. Available from: https://link.springer.com/article/10.1007/s00405-002-0458-x
30. Jiang B, Shi Y, Abou MB, Xu L, Liang G, Wei H. Effects of chronic intranasal dantrolene on nasal mucosa morphology in mice. Eur Rev Med Pharmacol Sci. 2022;26(1):198–203.
31. Xie F, Zhou X, Genter MB, Behr M, Gu J, Ding X. The Tissue-Specific Toxicity of Methimazole in the Mouse Olfactory Mucosa Is Partly Mediated through Target-Tissue Metabolic Activation by CYP2A5. Drug Metabolism and Disposition [Internet]. 2011 Jun 1 [cited 2022 Oct 26];39(6):947–51. Available from: https://dmd.aspetjournals.org/content/39/6/947