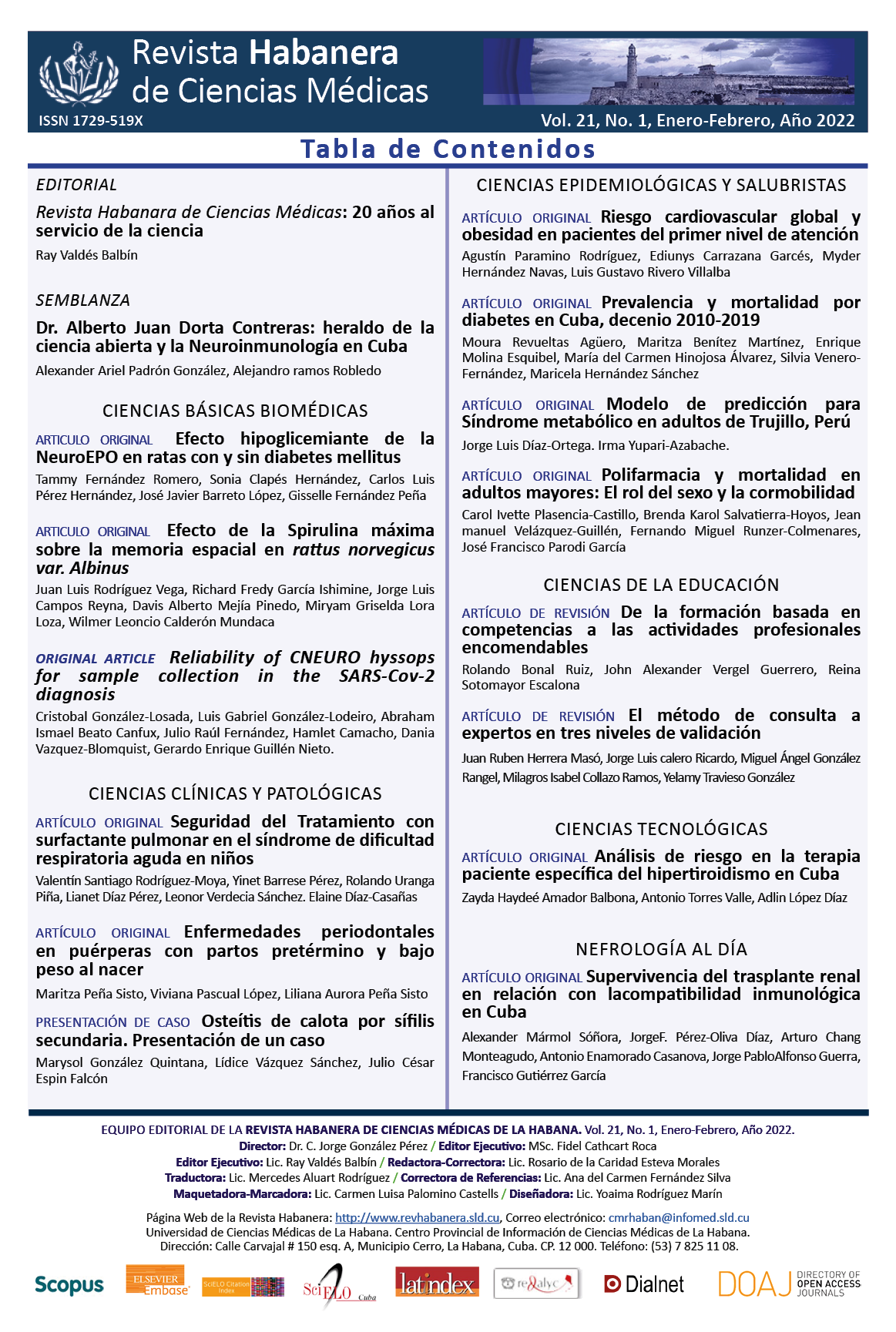
Polypharmacy and mortality in the elderly: the role of sex and comorbidity
Keywords:
Polypharmacy, mortality, elderly, comorbidity, sex.Abstract
Introduction: Polypharmacy is frequent in older adults. The association between polypharmacy and mortality is controversial due to the difficulty of controlling confounding factors such as comorbidity or gender.
Objective: The main objective of this study was to demonstrate the association between polypharmacy and mortality in older adults. The secondary objective wasto determine the role of sex and comorbidity on the association between polypharmacy and mortality.
Material and Methods: A retrospective, analytical, observational cohort study was conducted. A database of an outpatient geriatric clinic in a military hospital in Peru was analyzed. Outpatients ≥ 60 years of age were included. Polypharmacy was defined as the consumption of ≥ 5 drugs for ≥ 90 days. Cox regressions adjusted for age, marital status, cognitive impairment, physical frailty, functional dependence, and number of comorbidities were performed. Subgroup analyzes were performed for the risk of death from polypharmacy, stratified by sex and presence of comorbidity.
Results: Polypharmacy increased the risk of mortality. The Hazard Ratio adjusted for sex was 15,16 (1,80-21,66) and 5,55 (2,90-10,06) for women and men, respectively. The Hazard Ratio in non-comorbid patients was 1,94 (1,17-2,05; CI=95 %).
Conclusions: Polypharmacy is a risk factor for mortality regardless of the sex and comorbidities of the patient.Downloads
References
1. Fuster V. Changing Demographics. J Am Coll Cardiol [Internet]. 2017;69(24):3002-5. Disponible en: http://dx.doi.org/10.1016/j.jacc.2017.05.013
2. Russo J, Klein A. La tercera edad en Latinoamérica y México. Un largo transitar entre la ciudadanía y las subciudadanías. Forum Rev Dep Cienc Política [Internet]. 2020;(18):145-65. Disponible en: https://doi.org/10.15446/frdcp.n18.79546
3. Masnoon N, Kalisch Ellett L, Shakib S, Caughey GE. Predictors of Mortality in the Older Population: The Role of Polypharmacy and Other Medication and Chronic Disease-Related Factors. Drugs Aging [Internet]. 2020;37(10):767-76. Disponible en: https://doi.org/10.1007/s40266-020-00794-7
4. Muth C, Blom JW, Smith SM, Johnell K, Gonzalez Gonzalez AI, Nguyen TS, et al. Evidence supporting the best clinical management of patients with multimorbidity and polypharmacy: a systematic guideline review and expert consensus. J Intern Med [Internet]. 2018 [Citado 20/11/2021];285:272-88. Disponible en: https://onlinelibrary.wiley.com/doi/epdf/10.1111/joim.12842
5. Gómez Aguirre N, Caudevilla Martínez A, Bellostas Muñoz L, Crespo Avellana M, Velilla Marco J, Díez Manglano J. Pluripatología, polifarmacia, complejidad terapéutica y uso adecuado de la medicación. Rev Clínica Esp [Internet]. 2017;217(5):289-95. Disponible en: http://dx.doi.org/10.1016/j.rce.2016.12.013
6. Masnoon N, Shakib S, Kalisch Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr [Internet]. 2017 [Citado 20/11/2021];17(1):230. Disponible en: https://bmcgeriatr.biomedcentral.com/track/pdf/10.1186/s12877-017-0621-2.pdf
7. Castro Rodríguez JA, Orozco Hernández JP, Marín Medina DS. Polifarmacia y prescripción de medicamentos potencialmente no apropiados en ancianos. Revista Médica de Risaralda. 2016;21(2):52-7.
8. Chang TI, Park H, Kim DW, Jeon EK, Rhee CM, Kalantar Zadeh K, et al. Polypharmacy, hospitalization, and mortality risk: a nationwide cohort study. Sci Rep [Internet]. 2020;10(1):[Aprox. 2 p.]. Disponible en: https://doi.org/10.1038/s41598-020-75888-8
9. Leelakanok N, Holcombe AL, Lund BC, Gu X, Schweizer ML. Association between polypharmacy and death: A systematic review and meta-analysis. J Am Pharm Assoc [Internet]. 2017 [Citado 20/11/2021];57(6):729-738.e10. Disponible en: http://dx.doi.org/10.1016/j.japh.2017.06.002
10. Schöttker B, Saum KU, Muhlack DC, Hoppe LK, Holleczek B, Brenner H. Polypharmacy and mortality: new insights from a large cohort of older adults by detection of effect modification by multi-morbidity and comprehensive correction of confounding by indication. Eur J Clin Pharmacol [Internet]. 2017;73(8):1041-8. Disponible en: https://doi.org/10.1007/s00228-017-2266-7
11. Runzer Colmenares FM, Samper Ternent R, Al Snih S, Ottenbacher KJ, Parodi JF, Wong R. Prevalence and factors associated with frailty among Peruvian older adults. Arch Gerontol Geriatr [Internet].2014;58(1):69-73. Disponible en: https://doi.org/10.1016/j.archger.2013.07.005
12. McIsaac DI, MacDonald DB, Aucoin SD. Frailty for Perioperative Clinicians: A Narrative Review. Anesth Analg [Internet]. 2020 [Citado 20/11/2021];130(6):1450-60. Disponible en: https://journals.lww.com/anesthesia-analgesia/fulltext/2020/06000/frailty_for_perioperative_clinicians__a_narrative.3.aspx
13. Li R, Chen Y, Lv J, Liu L, Zong S, Li H, et al. Anxiety and related factors in frontline clinical nurses fighting COVID-19 in Wuhan. Medicine (Baltimore) [Internet]. 2020;99(30):e21413. Disponible en: http://dx.doi.org/10.1097/MD.0000000000021413
14. Bosello O, Donataccio MP, Cuzzolaro M. Obesity or obesities? Controversies on the association between body mass index and premature mortality. Eat Weight Disord - Stud Anorex Bulim Obes. 2016;21(2):165-74.
15. Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M. Defining Comorbidity: Implications for Understanding Health and Health Services. Ann Fam Med [Internet].2009;7(4):357-63. Disponible en: https://doi.org/10.1370/afm.983
16. Cruz Jentoft AJ, Bahat G, Bauer J, Boirie Y, Cooper C, Landi F, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age and Ageing [Internet]. 2019;48(1):16-31. Disponible en: https://doi.org/10.1093/ageing/afy169
17. Sandival Ampuero GA, Runzer Colmenares FM, Parodi JF. Functional assessment as a predictor of cognitive impairment: a retrospective cohort study. Medwave. 2017;17(09):7099.
18. Altuna Venegas S, Aliaga Vega R, Maguiña JL, Parodi JF, Runzer Colmenares FM. Risk of community-acquired pneumonia in older adults with sarcopenia of a hospital from Callao, Peru 2010–2015. Arch Gerontol Geriatr [Internet]. 2019;82:[Aprox. 2 p.]. Disponible en: https://doi.org/10.1016/j.archger.2019.01.008
19. Runzer Colmenares FM, Urrunaga Pastor D, Aguirre LG, Reategui Rivera CM, Parodi JF, Taype Rondan A. Frailty and vulnerability as predictors of radiotoxicity in older adults: A longitudinal study in Peru. Med Clínica Engl Ed [Internet]. 2017;149(8):325-30. Disponible en: http://dx.doi.org/10.1016/j.medcli.2017.02.022
20. Tinitana Ortega J, Torres Jaramillo I, Tacuri Romero J, Agila Vacacela J, Zari Espinoza D, Zhuzhingo Vásquez C. Polifarmacia en pacientes adultos mayores pluripatológicos que acuden al primer nivel de atención en salud. Facsalud-Unemi. 2019;2(3):34-41.
21. Arauz A, Serrano F, Ameriso SF, Pujol Lereis V, Flores A, Bayona H, et al. Sex Differences Among Participants in the Latin American Stroke Registry. J Am Heart Assoc [Internet]. 2020 [Citado 20/11/2021];9(4):[Aprox. 2p.]. Disponible en: https://www.ahajournals.org/doi/10.1161/JAHA.119.013903
22. Potter K, Flicker L, Page A, Etherton Beer C. Deprescribing in Frail Older People: A Randomised Controlled Trial. PLOS ONE [Internet]. 2016;11(3):e0149984. Disponible en: https://doi.org/10.1371/journal.pone.0149984
23. Reeve E, Jordan V, Thompson W, Sawan M, Todd A, Gammie TM, et al. Withdrawal of antihypertensive drugs in older people. Cochrane Database Syst Rev [Internet]. 2020 [Citado 20/11/2021];(6):[Aprox. 2 p.]. Disponible en: http://doi.wiley.com/10.1002/14651858.CD012572.pub2
24. Ramírez Pérez AR, Furones Mourelle JA, Ramos Cedeño AM. Deprescripción en el anciano polimedicado. Una mirada reflexiva en el contexto cubano. Rev haban cienc méd [Internet]. 2020 [Citado 20/11/2021];19(3):e3416. Disponible en: http://www.revhabanera.sld.cu/index.php/rhab/article/view/3416
25. García Orihuela M, Suárez Martínez R, Pérez Hernández B. Criterios STOPP-START y la prescripción inapropiada del anciano. Rev haban cienc méd [Internet]. 2020 [Citado 20/11/2021];19(6):e3765. Disponible en: http://www.revhabanera.sld.cu/index.php/rhab/article/view/3765
26. Proietti M, Raparelli V, Olshansky B, Lip GYH. Polypharmacy and major adverse events in atrial fibrillation: observations from the AFFIRM trial. Clin Res Cardiol [Internet]. 2016;105(5):412-20.Disponible en: https://doi.org/10.1007/s00392-015-0936-y
27. Chen LJ, Trares K, Laetsch DC, Nguyen TNM, Brenner H, Schöttker B. Systematic Review and Meta-Analysis on the Associations of Polypharmacy and Potentially Inappropriate Medication With Adverse Outcomes in Older Cancer Patients. J Gerontol A Biol Sci Med Sci [Internet]. 2021 [Citado 20/11/2021];76(6):1044-52. Disponible en: https://doi.org/10.1093/gerona/glaa128