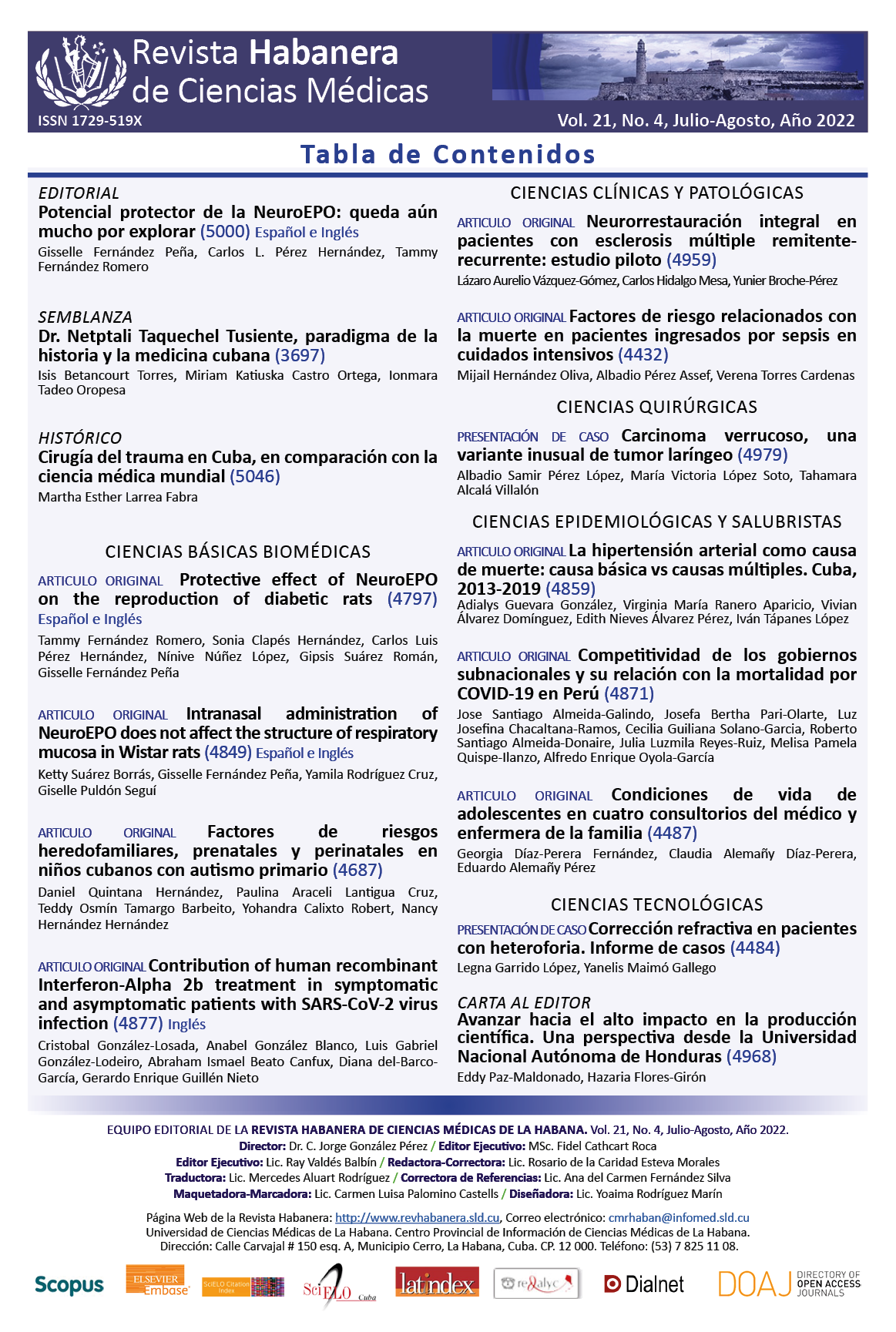
Competitiveness of subnational governments and their relationship with COVID-19 mortality in Peru
Keywords:
coronavirus infections, pandemics, collective effects of health disparities, mortality.Abstract
Introduction: The COVID-19 pandemic has revealed high disparities in the world population.
Objective: To describe the correlation between competitiveness and mortality from COVID-19 in Peru, with subnational governments as an element of study.
Material and Methods: Observational study based on the secondary analysis of deaths from COVID-19 that occurred in 2020 and the regional competitiveness index of subnational governments in 2019. The crude and standardized rates, the effect index, the difference and ratio of crude and standardized rates, the population attributable risk, the inequality gradient, and the relative and absolute gaps in mortality from COVID-19 were calculated.
Results: In 2020, the standardized mortality rate for COVID-19 (COVID-19-SMR) was 267,61 deaths per 105 inhabitants. Additionally, 21,53 % of the variance from the COVID-19-SMR is explained by the regional competitiveness index 2019 (p= 0,019); the slope inequality index was 29,68 and, for each point in the INCORE 2019, the COVID-19-SMR increased 100,78 points (R2a= 0,181). In quintile 1 of regional competitiveness, it was 151,83, while in quintile 5 it reached 449,15. The absolute inequality gap between both quintiles was 297,32 and it reached 2,95 in the relative inequality gap. The concentration curve evidenced the socio-geographic inequality of deaths from COVID-19 in 2020.
Conclusions: Mortality increased as subnational governments became more competitive, evidencing the socio-geographical inequality of the impact of the COVID-19 pandemic.
Downloads
References
1. Etienne CF. Health inequity continues to fuel COVID-19 pandemic and prolongs the efforts to end it [Internet]. Pan American Health Organization. 2021 [cited 2022 Jan 22]. Available from: https://www.paho.org/en/news/22-9-2021-health-inequity-continues-fuel-covid-19-pandemic-and-prolongs-efforts-end-it
2. Paremoer L, Nandi S, Serag H, Baum F. Covid-19 pandemic and the social determinants of health. BMJ [Internet]. 2021 Jan 29 [cited 2022 Jan 22];372(129):1–5. Available from: https://www.bmj.com/content/372/bmj.n129
3. Benach J, Friel S, Houweling T, Labonte R, Muntaner C, Schrecker T, et al. A conceptual framework for action on the social determinants of health [Internet]. World Health Organization Geneva. Geneva: World Health Organization; 2010 [cited 2022 Jan 19]. Available from: https://www.who.int/sdhconference/resources/ConceptualframeworkforactiononSDH_eng.pdf
4. Vera R. Competitividad en el Perú: situación y agenda pendiente. Moneda [Internet]. 2011 Nov [cited 2022 Jan 17];149(2):8–12. Available from: https://www.bcrp.gob.pe/docs/Publicaciones/Revista-Moneda/moneda-149/moneda-149-02.pdf
5. Tapia JA. Crecimiento económico e inequidades en salud. Rev Peru Med Exp Salud Publica [Internet]. 2013 Dec [cited 2022 Jan 22];30(4):657–64. Available from: https://www.scielosp.org/article/ssm/content/raw/?resource_ssm_path=/media/assets/rpmesp/v30n4/a19v30n4.pdf
6. Benzaquen J, Alfonso del Carpio L, Alberto Zegarra L, Alberto Valdivia C. A competitiveness index for the regions of a country. Cepal Review [Internet]. 2010 Dec [cited 2022 Jan 17];67–84. Available from: http://www.imd.ch/documents/wcc/content/Fundamentals.pdf
7. De-la-Torre-Ugarte-Guanilo M, Oyola-García A. Los determinantes sociales de la salud: una propuesta de variables y marcadores/indicadores para su medición. Revista Peruana de Epidemiología [Internet]. 2014 [cited 2022 Jan 17];18(1):1–6. Available from: https://www.redalyc.org/pdf/2031/203132677002.pdf
8. Mo Q, Chen X, Yu B, Ma Z. Levels of economic growth and cross-province spread of the COVID-19 in China. J Epidemiol Community Health [Internet]. 2021 Sep 1 [cited 2022 Jan 22];75(9):824–8. Available from: https://jech.bmj.com/content/75/9/824
9. Aycock L, Chen X. Levels of economic developement and the spread of coronavirus disease 2019 (COVID-19) in 50 U.S. states and territories and 28 European countries: an association analysis of aggregated data. Global Health Journal [Internet]. 2021 Mar 1 [cited 2022 Jan 22];5(1):24–30. Available from: https://www.sciencedirect.com/science/article/pii/S2414644721000063?utm_source=TrendMD&utm_medium=cpc&utm_campaign=Global_Health_Journal_TrendMD_1
10. Cieza J, Uriol C. Letalidad y la mortalidad de Covid 19 en 60 países afectados y su impacto en los aspectos demográficos, económicos y de salud. Rev Med Hered [Internet]. 2020 [cited 2022 Jan 31];31:214–21. Available from: http://www.scielo.org.pe/pdf/rmh/v31n4/1729-214X-rmh-31-04-214.pdf
11. Office of National Statistics. Deaths involving COVID-19 by local area and socioeconomic deprivation - Office for National Statistics [Internet]. ONS. 2020 [cited 2022 Jan 22]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsinvolvingcovid19bylocalareasanddeprivation/deathsoccurringbetween1marchand31july2020
12. Karlinsky A, Kobak D. Tracking excess mortality across countries during the covid-19 pandemic with the world mortality dataset. Elife [Internet]. 2021 Jun 1 [cited 2022 Jan 6];10:e69336. Available from: https://elifesciences.org/articles/69336
13. Organización Mundial de la Salud. WHO Coronavirus (COVID-19) Dashboard [Internet]. OMS. 2021 [cited 2022 Jan 6]. Available from: https://covid19.who.int/table
14. Villarán F, Ramos M, Quintanilla P, Solari L, Ñopo H, Álvarez I. Informe sobre las causas del elevado número de muertes por la pandemia del COVID-19 en el Perú [Internet]. Lima: CONCYTEC; 2021 [cited 2022 Jan 6]. Available from: www.gob.pe/concytec
15. Ministerio de Salud del Perú. Fallecidos por COVID-19 [Internet]. Plataforma Nacional de Datos Abiertos. 2022 [cited 2022 Jan 15]. Available from: https://www.datosabiertos.gob.pe/dataset/fallecidos-por-covid-19-ministerio-de-salud-minsa
16. Instituto Peruano de Economía. Índice de competitividad regional (INCORE): Metodología [Internet]. 2022 [cited 2022 Jan 15]. Available from: https://incoreperu.pe/portal/index.php/metodologia
17. Ministerio de Salud del Perú. Estadísticas de población [Internet]. REUNIS: Repositorio Único Nacional de Información en Salud. 2022 [cited 2022 Jan 15]. Available from: https://www.minsa.gob.pe/reunis/data/poblacion_estimada.asp
18. Organización Panamericana de la Salud. Lineamientos básicos para el análisis de la mortalidad [Internet]. Washington D.C.: OPS; 2017 [cited 2022 Jan 15]. Available from: https://iris.paho.org/bitstream/handle/10665.2/34492/9789275319819-spa.pdf?sequence=7
19. Surveillance Epidemiology and End Results Program. Datasets - Standard population Data: World (WHO 2000-2025) Standard [Internet]. 2013 [cited 2022 Jan 15]. Available from: https://seer.cancer.gov/stdpopulations/world.who.html
20. Instituto Peruano de Economía. Base de datos: INCORE Edición 2019 - Actualización [Internet]. 2019 [cited 2022 Jan 15]. Available from: https://incoreperu.pe/portal/index.php/databank
21. Vera CP, Rendon S. Is the Global Competitiveness Index a reliable tool for the design of labor market policies? Evidence from Peru. Policy Paper Series [Internet]. 2021 Sep [cited 2022 Jan 31];180. Available from: https://docs.iza.org/pp180.pdf
22. Flores A. Competitividad y desigualdad en América Latina [Internet]. Consumo y ciudadanía. 2020 [cited 2022 Jan 31]. Available from: https://consumoyciudadania.org/competitividad-y-desigualdad-en-america-latina/
23. Liang CK, Chen LK. National health care quality and COVID-19 case fatality rate: International comparisons of top 50 countries. Arch Gerontol Geriatr [Internet]. 2022 Jan 1 [cited 2022 Jan 31];98:104587. Available from: https://pubmed.ncbi.nlm.nih.gov/34839063/
24. Dirección General de Medicamentos Insumos y Drogas. Gasto de bolsillo en salud y medicamentos. Periodo 2012-2019 [Internet]. Primera. Medrano A, Alcántara J, Machaca N, Mendoza R, editors. Dirección General de Medicamentos, Insumos y Drogas. Lima: Ministerio de Salud; 2021 [cited 2022 Jan 31]. Available from: http://repositorio.digemid.minsa.gob.pe/xmlui/handle/DIGEMID/191
25. Hernández-Vásquez A, Rojas-Roque C, Santero M, Prado-Galbarro FJ, Roselli D. Gasto de bolsillo en salud en adultos mayores peruanos: análisis de la Encuesta Nacional de Hogares sobre Condiciones de Vida y Pobreza 2017. Revista Peruana de Medicina Experimental y Salud Pública [Internet]. 2018 [cited 2022 Feb 2];35(3):390–9. Available from: https://rpmesp.ins.gob.pe/rpmesp/article/view/3815/3116
26. Tarrillo D, Zavala J, Quequezana P, Gómez L, Najarro D, Castro V, et al. Informe de calidad del gasto público en salud 2019 [Internet]. Zacnich R, editor. Lima: COMEXPERU - Sociedad de Comercio Exterior del Perú; 2019 [cited 2022 Jan 31]. Available from: https://www.comexperu.org.pe/upload/articles/reportes/informe-calidad-001.pdf
27. United Nations. Policy Brief: COVID-19 and Universal Health Coverage [Internet]. Nueva York: UN; 2020 [cited 2022 Feb 2]. Available from: https://unsdg.un.org/sites/default/files/2020-10/SG-Policy-Brief-on-Universal-Health-Coverage_English.pdf
28. Instituto Peruano de Economía. Índice de Competitividad Regional 2019 [Internet]. Lima: IPE; 2019 [cited 2022 Jan 31]. Available from: https://incoreperu.pe/portal/images/financepress/ediciones/INCORE_2019_FINAL.pdf
29. Durand D. Población afiliada a algún seguro de salud [Internet]. Lima: INEI; 2018 [cited 2022 Feb 2]. Available from: www.inei.gob.pe