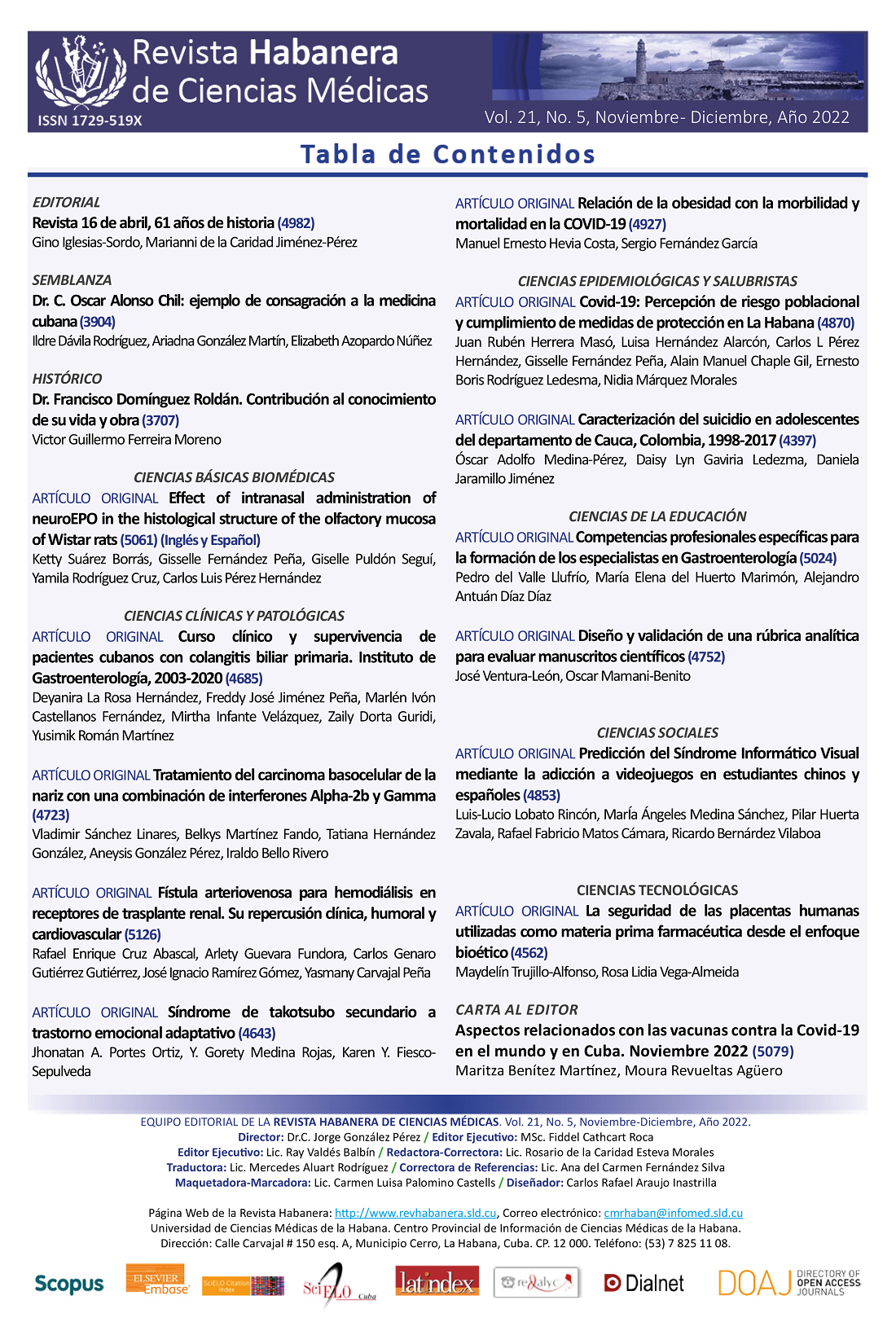
Clinical course and response to treatment of Cuban patients with primary biliary cholangitis. Institute of Gastroenterology, 2003-2020
Keywords:
primary biliary cholangitis, cirrhosis, survival, rate of complications, symptomatic presentation.Abstract
Introduction: Primary biliary cholangitis (PBC) is a cholestatic liver disease. The natural history and prognosis of PBC has been difficult to characterize. In Latin America and the Caribbean, there are very few research works on the subject.
Objective: To describe the clinical and developmental characteristics and survival of patients with PBC.
Material and Methods: Descriptive, longitudinal and ambispective study of patients older than 18 years with a diagnosis of PBC, treated at the Institute of Gastroenterology between September 2003 and January 2020. Demographic, clinical, biochemical and histological variables were evaluated from the data of medical records. For data processing, the statistical package SPSS version 21,0 was used.
Results: A total of 45 patients were included, most of them female (95 %) and with symptomatic presentation (55,6 %). In addition, 71,1 % of the patients presented some complications, cirrhosis being the most frequent; in 28,8 % of the cirrhotic patients, there were complications secondary to liver injury, predominantly ascites, followed by variceal digestive bleeding, encephalopathy, hepatocellular carcinoma (HCC), and bacterial infections associated with cirrhosis. Cumulative survival exceeded 95 % at five years.
Conclusions: The survival of patients with PBC was high over time despite the high rate of complications.
Downloads
References
1. European Association for the Study of the Liver. EASL Clinical Practice Guidelines: The diagnosis and management of patients with primary biliary cholangitis. J Hepatol [Internet]. 2017 [Citado17/12/2021];67(1):145-72. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/28427765
2. Gazda J, Drazilova S, Janicko M, Grgurevic I, Filipec Kanizaj T, Koller T, et al. Prognostic Factors in Primary Biliary Cholangitis: A Retrospective Study of Joint Slovak and Croatian Cohort of 249 Patients. J Pers Med [Internet]. 2021 [Citado17/12/2021];11(6):[Aprox. 2 p.]. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/34205918
3. Floreani A, Mangini C. Primary biliary cholangitis: Old and novel therapy. Eur J Intern Med [Internet]. 2018 [Citado17/12/2021];47:1-5. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/28669591
4. Cheung KS, Seto WK, Fung J, Lai CL, Yuen MF. Epidemiology and Natural History of Primary Biliary Cholangitis in the Chinese: A Territory-Based Study in Hong Kong between 2000 and 2015. Clin Transl Gastroenterol [Internet]. 2017 [Citado17/12/2021];8(8):e116. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/28858291
5. Onofrio FQ, Hirschfield GM, Gulamhusein AF. A Practical Review of Primary Biliary Cholangitis for the Gastroenterologist. Gastroenterol Hepatol [Internet]. 2019 [Citado17/12/2021];15(3):145-54. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/31061656
6. Fernández MIC, Hernández DR, Cabrera Eugenio DE, Palanca W, Guridi ZD, González Fabián L. Diagnosis and Treatment of Autoimmune Liver Diseases in a Tertiary Referral Center in Cuba. Curr Ther Res Clin Exp [Internet]. 2017 [Citado 17/01/21];85:8-14. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/29158853
7. González Huezo MS, Delgado Ayala LY, Osorio Núñez AL, Meléndez Mercado C. Autoimmune associations in a Mexican cohort with primary biliary cholangitis. Rev Gastroenterol Mex [Internet]. 2019 [Citado17/12/2021]; 84(2):130-5. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/30017344
8. Levy C, Naik J, Giordano C, Mandalia A, O'Brien C, Bhamidimarri KR, et al. Hispanics with primary biliary cirrhosis are more likely to have features of autoimmune hepatitis and reduced response to ursodeoxycholic acid than non-Hispanics. Clin Gastroenterol Hepatol [Internet]. 2014 [Citado 17/01/2021]; 12(8):1398-405. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/24361417
9. Carbone M, Nardi A, Flack S, Carpino G, Varvaropoulou N, Gavrila C, et al. Pretreatment prediction of response to ursodeoxycholic acid in primary biliary cholangitis: development and validation of the UDCA Response Score. Lancet Gastroenterol Hepatol [Internet]. 2018 Sep [Citado17/12/2021];3(9):626-34. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/30017646
10. Chapman RW. Cost effectiveness of using ursodeoxycholic acid to treat primary biliary cholangitis. Br J Hosp Med [Internet]. 2018 Aug [Citado17/12/2021];79(8):460-4. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/30070957
11. Corpechot C, Chazouilleres O, Poupon R. Early primary biliary cirrhosis: biochemical response to treatment and prediction of long-term outcome. J Hepatol [Internet]. 2011 Dec [Citado17/12/2021]; 55(6):1361-7. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/21703194
12. Gatselis NK, Goet JC, Zachou K, Lammers WJ, Janssen HLA, Hirschfield G, et al. Factors Associated With Progression and Outcomes of Early Stage Primary Biliary Cholangitis. Clin Gastroenterol Hepatol [Internet]. 2020 Mar [Citado17/12/2021];18(3):684-92. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/31419573
13. Wilde AB, Lieb C, Leicht E, Greverath LM, Steinhagen LM, Wald de Chamorro N, et al. Real-World Clinical Management of Patients with Primary Biliary Cholangitis-A Retrospective Multicenter Study from Germany. J Clin Med [Internet]. 2021 [Citado17/01/2021];10(5):[Aprox. 3 p.]. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/33806503
14. Cheung AC, Lammers WJ, Murillo Perez CF, Van Buuren HR, Gulamhusein A, Trivedi PJ, et al. Effects of Age and Sex of Response to Ursodeoxycholic Acid and Transplant-free Survival in Patients With Primary Biliary Cholangitis. Clin Gastroenterol Hepatol [Internet]. 2019 [Citado17/12/2021];17(10):2076-84. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/30616022
15. Lindor KD, Gershwin ME, Poupon R, Kaplan M, Bergasa NV, Heathcote EJ, et al. Primary biliary cirrhosis. Hepatology [Internet]. 2009 [Citado17/12/2021];50(1):291-308. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/19554543
16. Cordell HJ, Han Y, Mells GF, Li Y, Hirschfield GM, Greene CS, et al. International genome-wide meta-analysis identifies new primary biliary cirrhosis risk loci and targetable pathogenic pathways. Nat Commun [Internet]. 2015 [Citado17/12/2021];6:8019. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/26394269
17. Prince MI, Chetwynd A, Craig WL, Metcalf JV, James OF. Asymptomatic primary biliary cirrhosis: clinical features, prognosis, and symptom progression in a large population based cohort. Gut [Internet]. 2004 [Citado17/12/2021];53(6):865-70. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/15138215
18. Llorente AM, Barraza Ortiz D, Ramos Aguilar G, Mejía Loza S. Colangitis biliar primaria. Rev Hosp Juan Mex. 2019;86(4):188-95.
19. Kaps L, Grambihler A, Yemane B, Nagel M, Labenz C, Ploch P, et al. Symptom Burden and Treatment Response in Patients with Primary Biliary Cholangitis (PBC). Dig Dis Sci [Internet]. 2020 [Citado17/12/2021];65(10):3006-13. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/31853781
20. Crosignani A, Battezzati PM, Invernizzi P, Selmi C, Prina E, Podda M. Clinical features and management of primary biliary cirrhosis. World journal of gastroenterology [Internet]. 2008 Jun [Citado17/12/2021];14(21):3313-27. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/18528929
21. Rodríguez Lugo DA, Coronado Tovar JJ, Solano Villamarin GA, Otero Regino W. Colangitis biliar primaria. Parte 2. Actualización: diagnóstico, enfermedades asociadas, tratamiento y pronóstico. Revista de Gastroenterología del Perú [Internet]. 2018 [Citado17/12/2021];38:64-71. Disponible en: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1022-51292018000100010&nrm=iso
22. Yerragorla P, Shady A, Bergasa NV. Characterization of patients with primary biliary cholangitis and autoimmune hepatitis from a community hospital in East Harlem. Arch Clin Gastroenterol. 2020;6(1).
23. Corpechot C, Carrat F, Bahr A, Chretien Y, Poupon RE, Poupon R. The effect of ursodeoxycholic acid therapy on the natural course of primary biliary cirrhosis. Gastroenterology [Internet]. 2005 Feb [Citado17/12/2021];128(2):297-303. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/15685541
24. Álvaro D, Carpino G, Craxi A, Floreani A, Moschetta A, Invernizzi P. Primary biliary cholangitis management: controversies, perspectives and daily practice implications from an expert panel. Liver Int [Internet]. 2020 [Citado17/12/2021];40(11):2590-601. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/32757367
25. To U, Silveira M. Overlap Syndrome of Autoimmune Hepatitis and Primary Biliary Cholangitis. Clin Liver Dis [Internet]. 2018 [Citado17/12/2021];22(3):603-11. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/30259856
26. Yoo JJ, Cho EJ, Lee B, Kim SG, Kim YS, Lee YB, et al. Prognostic Value of Biochemical Response Models for Primary Biliary Cholangitis and the Additional Role of the Neutrophil-to-Lymphocyte Ratio. Gut Liver [Internet]. 2018 [Citado 15/12/21];12(6):714-21. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/30400732
27. Murillo Pérez CF, Hirschfield GM, Corpechot C, Floreani A, Mayo MJ, Van der Meer A, et al. Fibrosis stage is an independent predictor of outcome in primary biliary cholangitis despite biochemical treatment response. Aliment Pharmacol Ther [Internet]. 2019 [Citado17/12/2021];50(10):1127-36. Disponible en: http://www.ncbi.nlm.nih.gov/pubmed/31621931
28. Örnolfsson LS, Olafsson S, Bergmann O, Björnsso E. Biochemical response to ursodeoxycholic acid among PBC patients: a nationwide population- based study. Scandinavian journal of gastroenterology. 2019;54(5):609-16.